15 Jun 2020
It is common to find it difficult to eat after critical illness and maintain a healthy weight. This information tells you about the nutrition to have at home and how to help with common problems you may have with eating. You can click the tabs above to access each section.
This information forms part of advice on "Nutrition and recovery after critical illness’, so also see the ‘Nutrition when in the hospital’ and 'Tips to help with some common problems with eating' information.
Introduction
Leaving hospital after critical illness is a big step forward in your recovery. It is great that you are well enough to go home, but you might find that there are some things you find difficult. It may take some time to get back to a normal life, and things that used to be easy, seem difficult, such as being able to eat and drink like you used to.
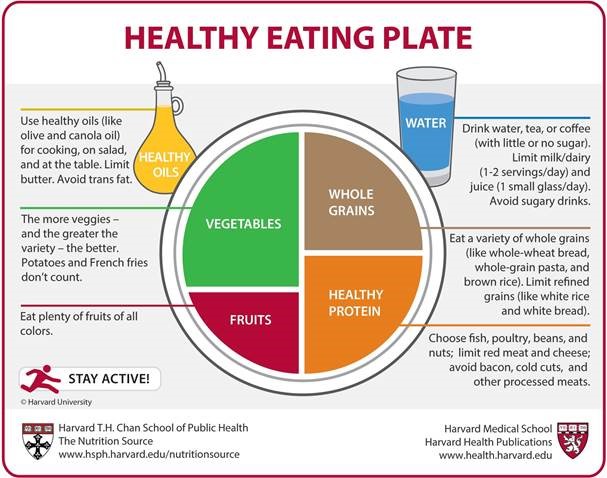
Your body has been through a lot and it now needs the right food and drink to help your recovery. Eating well helps you to:
- have more energy as you begin to do more
- feel less tired
- avoid losing any more weight
- re-build muscle
- heal
- fight infection and have a strong immune system
- be able to deal with any side effects of any treatment you may still be having.
This information gives you information about what can help you with eating in this stage of your recovery at home.
This information is part of a series of information about nutrition and recovery after critical illness. The other information sheets are about nutrition when in hospital and tips to help with some common problems with eating. Nutrition is the term used to describe what you eat or drink to give you energy and other nutrients to help your body recover and stay healthy.
Having this information may help you to understand more about nutrition, how it can help your recovery and overcome any difficulties with eating after your critical illness. We hope it will help you and your family, but if you have any particular nutritional questions or worries, please ask your doctor for help or ask if they can refer you to a dietitian. A dietitian is a registered health care professional who advises about nutrition for health and during illness.
You can check how healthy your current weight is for your height on the NHS website.
There are also very good self-screening tools to use to check whether you should be worried about how your low weight or poor eating may affect your health, from the Patients Association and the British Association of Parenteral and Enteral Nutrition.
If you have ongoing difficulties with eating, even after this advice, if you have a low weight or are continuing to lose weight or strength, do speak to your doctor or ask to see a dietitian.